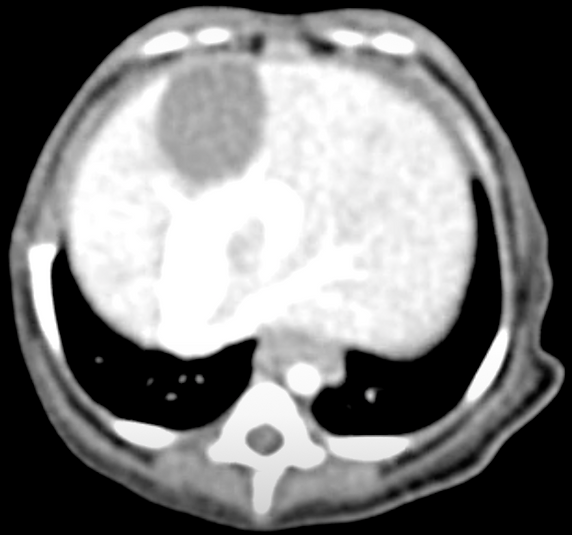
Intrahepatic portosystemic shunt
Normally, all of the blood that come from the intestines flows directly to the liver so the liver is able to process toxins coming from the intestinal tract. Shunts occur when there is a direct communication between the blood coming from the intestines (portal circulation) and the systemic circulation (caudal vena cava). This is a congenital abnormality. Shunts can be classified as extrahepatic (where the communication occurs outside of the liver) or intrahepatic (communication occurs within the liver).

The treatment that provides the best outcome is to correct the shunting vessel. Unfortunately, this is challenging to do in intrahepatic shunts since the surgeon would have to dissect the liver, which has been associated with many complications. Surgical approaches for IHPSSs have been associated with complication rates as high as 77%, perioperative mortality rates as high as 64%. This prompted the need of developing alternative treatment options for these patients.
A CT scan is necessary prior to the endovascular procedure in order to map the shunting vessel. Then, a separate procedure will be scheduled for the endovascular procedure. This helps to minimize anesthesia time as well as intravenous contrast load. We recommend performing these procedures when patients are somewhere between 4-6 months of age. The risk in doing them when they are very young is that we don't want them to over their caval stent since vessel size may increase in diameter as they grow.

Gastrointestinal bleeding was initially noted in approximately 13% of dogs prior to endovascular treatment. The risk of gastrointestinal bleeding has decreased significantly after life-long omeprazole treatment has been recommended.

Endovascular techniques were developed to close the shunting vessel (i.e. decrease blood flow through the shunting vessel). This technique involves passing guidewires and catheters through the jugular vein (typically) and accessing the shunting vessel. Thrombogenic coils are placed within the shunting vessel to decrease flow. A stent in the caudal vena cava is placed in order to prevent the coils from migrating into the systemic circulation. Portal pressures are measured during the procedure to make sure that the coils are not significantly increasing portal pressures, which could be associated with gastrointestinal side-effects. Patients normally remain in the hospital for 1-2 days after the procedure. Possible intra-op complications are low, but can be due to portal hypertension, coil displacement, arrhythmias (if caval stent is placed within the right atrium - more of common with left divisional portosystemic shunts). Possible post-operative complications include seizures, hemorrhage from the jugular access site, and portal hypertension. Fortunately, these are not common complications.
Fluoroscopic video of percutaneous transjugular coil embolization (PTCE)

-
Catheterizing the shunting vessel
-
Measuring portal pressure
-
Measuring caudal vena cava diameter
-
Placement of caval stent
-
Catheterizing shunting vessel to monitor portal vein pressure
-
Inserting coils into shunting vessel
-
Contrast study post-coiling
Step-by-step
Radiograph post coiling procedure showing the caudal vena cava stent and coils within the shunting vessel.

Outcome of IHPSS coiling procedure
Overall, endovascular procedures have lower morbidity and mortality when compared to conventional surgical procedures. Outcome of endovascular procedures is considered excellent or fair in approximately 80% of patients. The median survival post-procedure is approximately 6 years. Most of the treated patients do well with one procedure (~85%). However, approximately15% may benefit from additional coils. There are 5% of dogs that have a high pressure gradient that do not require treatment. When evaluating outcome according to shunt location, excellent outcome was achieved in 80% of central divisional, 67% of right divisional, and 48% of left divisional intrahepatic shunts. Left divisional intrahepatic shunts are most cranially and most likely to develop collaterals.
If the coiling procedure is declined (Expectations for medical therapy)
Lastly, medical treatment can also be considered. However, survival with medical treatment has been considered very short for intrahepatic portosystemic shunts. In a study retrospective study, 17 dogs with congenital intrahepatic shunts had and mean survival time of 10.2 months +/- 9.5 months (standard deviation) (range: 1-31 months). Age at onset of clinical signs and low BUN were considered poor prognostic indicators in this group of dogs. The large caliber of these intrahepatic shunt vessels is thought to play a role in overall survival, when the shunting vessel is not addressed and signs only clinical signs are treated.